MLD & CDT FAQs
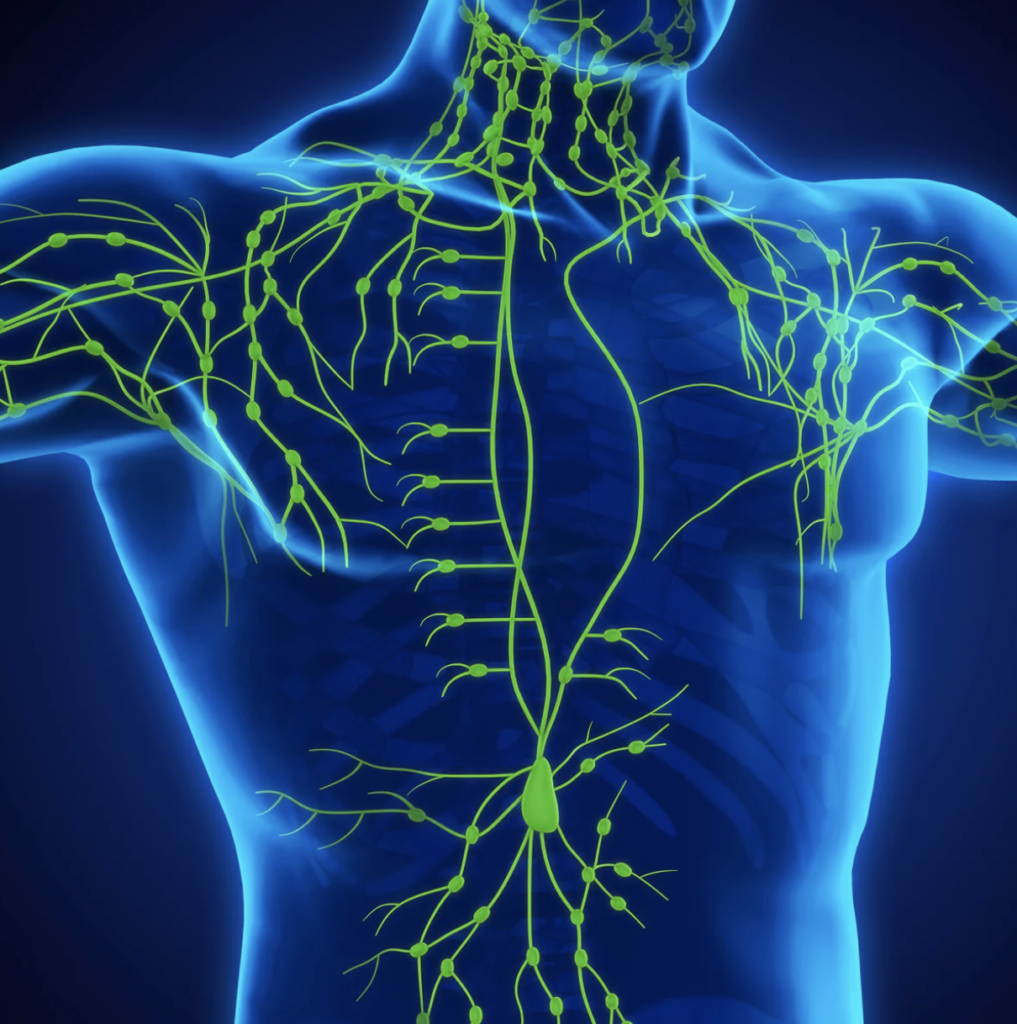
What is the Lymphatic System?
The lymphatic system is part of our immune system. It carries excess proteins, bacteria, waste and toxins to the lymph nodes where it is filtered and either expelled from the body or re-introduced to the bloodstream. The lymphatic system consists of tissues and organs, including bone marrow, thymus, lymph nodes and spleen, as well as the channels called lymph collectors, ducts and trunks, that carry lymph. There are lymph vessels and glands that comprise the lymphatic system and they are throughout the body similar to blood vessels. Many are found in the very superficial tissue of our skin, making Manual Lymphatic Drainage an effective way to influence the system.
What is Lymphedema?
The condition Lymphedema sets itself apart from other edemas/swelling by being high in protein molecules. Lymphedema is an abnormal buildup of protein-rich fluid in any part of the body as a result of malfunction in the lymphatic system. There are two main types of Lymphedema: primary or secondary Lymphedema. Primary lymphedema is usually evident at birth or before the age of 35. It can also manifest later in life. It is caused by hereditary malformation (faulty genes) of the lymph system. This type of lymphedema is rare, affecting approximately 1 in every 10,000 people. It is typically divided into three types: aplasia, hypoplasia and hyperplasia. This refers to where and how the lymphatic system is affected. Secondary lymphedema occurs as a result of damage to the lymphatic system, such as infection, injury, trauma, surgery, radiation, or cancer treatment. The most common causes in the U.S. are cancer treatments such as radiation or the removal of lymph nodes, both during biopsy and surgery. These may disrupt or damage the lymph system. Other causes are: chronic venous insufficiency, phlebolymphedema, obesity, and filariasis.
For additional information in Lymphedema visit: lymphoedema.org, lymphcare.com, lymphnet.org
What is MLD?
MLD or Manual Lymphatic Drainage, is a therapy that lightly stretches the skin to promote the movement of lymphatic fluid in a desired direction. It should not be confused with traditional massage you receive at a spa. MLD is very light touch on the skin and the target is the lymphatic system, not muscles, ligaments or tendons. In fact, most of the lymphatic system is above the muscle layer. MLD is indicated for fibromyalgia, chronic fatigue syndrome, chronic rheumatoid arthritis, swelling, water retention, sinus congestion, and constipation.
MLD therapy for lymphedema is applied to your unaffected areas first, making it possible for the fluid to move out of the affected area, or “decongest” it. An uncompromised lymphatic system that is receiving MLD for toxin removal, autoimmune benefits or similar goals, will not necessarily follow the same sequence as or lymphedema.
Deep abdominal breathing diaphragmatic techniques are done at the beginning and end of a therapy session to help open your deep lymphatic pathways. It’s very relaxing and helps increase movement of fluid toward your heart.
A Certified Lymphedema Therapist (CLT) who has been specially trained in MLD should perform this therapy for complex and compromised cases, such as lymphedema.
What does Lymphedema treatment include?
Complete decongestive therapy (CDT) aims to reduce your swelling, improve the condition of your skin, increase your mobility, reduce the risk of infection, and optimize your overall health.
This is the gold standard, most common and doctor recommended treatment for lymphedema. Prevention and controlling lymphedema play an important role with this condition since there is no cure. CDT has two phases. Phase 1: Decongestion (MLD, bandaging, exercise, skincare) and Phase 2: maintenance which includes home care (maintain results of phase 1 and gain long-term control of your lymphedema). Each phase includes variations of the following five components.
MLD, Manual Lymphatic Drainage. This uses special techniques to move protein-rich fluid into working lymph nodes, where they are then drained. It is crucial that this is done by a fully Certified Lymphedema Therapist (CLT) for patients with lymphedema. The therapist needs a thorough knowledge of the lymphatic system in order to properly protect the patient. The direction and location of the lymph vessels and draining is critical so as not to flood fluid into an already compromised region. Manual lymphatic drainage can also be done for a non-compromised lymphatic system. This can benefit immune function and help detox the body.
Compression bandaging. Unlike the heart pumping the blood through the circulatory system, the lymphatic system has no pump for lymph fluid. Breathing exercises and muscle movement are what cause lymphatic valves to open and close and move fluid through different vessels. Bandaging creates a specific pressure barrier that helps prevent fluid backlogging into compromised tissue by creating interstitial pressure that is beneficial for the lymphatic system to function.
Exercise. Light exercises while wearing compression bandages encourages movement of the lymph fluid out of the affected limb. It is important not to overdo it and follow the directions of your therapist and doctor.
Skin Care. This is of UTMOST importance to lymphedema. Waste levels are high under the edematous skin, the diffusion distance is greater making it more difficult for white blood cells to travel to fight infection and any small breakage can lead to complications such as cellulitis. Using low pH-level lotion and soaps are best. Lotions are always applied before bandaging. Meticulous nail care is also key, hangnails can be an easy place for infection.
Self-Care Management. Learning how to manage your lymphedema on your own is a key component in your treatment. Studies suggest that managing your symptoms, eating a healthy diet, controlling body weight and learning how to reduce injury to the area are important.
How can I begin complete decongestive therapy?
CDT can begin once you have a prescription from your doctor. It is important to see a therapist that has passed intensive training to treat lymphedema. You will see the initials CLT, certified lymphedema therapist, behind her/his name.
Are there Lymphedema risk reduction practices?
People who have had surgery to remove lymph nodes should be aware of those activities that put too much pressure on the affected limb near those lymph node regions. Protective measures to avoid injury and infection include:
Maintaining proper hygiene (clean the skin of the affected limb daily and apply lotion, when drying the limb, be gentle but thorough; take proper care of the fingernails and avoid cutting cuticles; clean all cuts with soap and water, apply antibacterial ointment and a sterile dressing)
Staying fit (do light exercises regularly to improve drainage, but first consult with your doctor; keep the limb elevated when possible)
Take precautions with everyday activities (avoid vigorous, repetitive movements against resistance, i.e. scrubbing, pulling, pushing with the limb; avoid sunburns and other burns to the affected limb; avoid razors when shaving, use an electric shaver instead)
Wearing the right attire: no clothing with elastic cuffs on an affected limb, no heavy bags or items carried on or by affected arms.
Speak up at the doctor’s office: make sure that all injections are given and blood tests are drawn in the unaffected limb, if possible have blood pressure tests done on the unaffected limb, avoid extreme hot or cold temperatures on the affected limb (i.e. heating pads or ice packs), notify your doctor immediately of any signs of infection, such as redness, pain, heat, increased swelling or fever.
Talk with your doctor about what you can do to try to prevent lymphedema. If lymphedema does develop, let your doctor know right away.
For more information on risk reduction practices, lymphedema alert bracelets and empowering the lymphedema community, please visit the National Lymphedema Network.